In recent years, there has been a shift in the healthcare landscape towards value-based care. This shift has led to an increase in the use of Remote Patient Monitoring (RPM) services. RPM is a type of telemedicine that allows healthcare providers to remotely monitor patients, by using technology.

RPM has a number of benefits for both patients and providers. For patients, it can improve outcomes and increase access to care. For providers, it can improve efficiency and reduce costs.
Despite these benefits, there are a number of challenges associated with RPM. One of the most significant challenges is Billing and Reimbursement. RPM services are not always covered by insurance companies, and when they are, the reimbursement rates are often low. This makes it difficult for providers to sustain an RPM program.
In this article, we will discuss the billing and reimbursement challenges associated with RPM. We will also provide some tips on how to overcome these challenges and maximize revenue for your RPM Program.
What is Remote Patient Monitoring (RPM)?
Remote Patient Monitoring (RPM) is a growing trend in healthcare, as it offers a more convenient and cost-effective way to care for patients. RPM refers to the use of technology to collect patient data from a remote location and then send it to a care team for review. This data includes things like vital signs, activity levels, and other health metrics.
RPM is particularly beneficial for patients who require frequent monitoring but do not need to be seen by a healthcare provider, in person. For example, RPM can be used to monitor patients with chronic conditions, such as heart disease or diabetes. It can also be used to check in on post-operative patients or those with mental health conditions.
There are many benefits of RPM, both for patients and healthcare providers. Patients can enjoy greater convenience and flexibility, while providers can reduce costs and improve patient care.
RPM can also improve healthcare outcomes. Studies have shown that patients who use RPM are more likely to take their medications as prescribed and have better health outcomes overall.

Remote Patient Monitoring Tools:
- Blood Pressure Cuffs.
- Calorie-Tracking Monitors.
- Glucose Meters.
- Heart Rate Monitors.
- Oximeters.
- Musculoskeletal Risk Stratification Equipment.
- Grip Strength Sensors.
The use of monitoring tools will differ based on the physical condition of the patients and the disease they suffer. Remote Healthcare Monitoring tools prevent patients from being in a long-term care facility and physicians enjoy the comfort of monitoring patient’s conditions even if they are distant from them. their condition with devices away from their office. Most Americans widely use smart devices for personal care.
Coverage of Remote Patient Monitoring:
Medical Insurance covers almost 90% of RPM systems in the USA. Remote Patient Monitoring is covered by Medicare and Medicaid. After the Covid – 19 pandemic, commercial insurance payers are now covering RPM in their insurance plans.
How Patients Qualify for RPM:
The Covid-19 pandemic created an urge for physicians and healthcare to concentrate more on remote patient monitoring systems, and to extend the care for Chronic and Acute conditions. Patients with the following Chronic and Acute conditions are eligible for RPM based on the suggestion by the physicians.
Chronic Conditions:
Through RPM, Physicians can effectively monitor patients with Chronic Conditions such as Diabetes, Dementia, Hypertension, Congestive Heart Failure, Obesity, COPD, and Behavioral Health.
Regular monitoring of patients with these conditions ensures that they are in good health and that any deterioration is observed quickly and a prompt medical response is delivered to save lives.
RPM also helps the medical teams to equip with the devices for unexpected medical events based on the patient’s history and take good care of them.
Acute Conditions:
Heart Attacks, Severe Burns, Flu, Pneumonia, Respiratory Infections, Bronchitis, and injuries with limited mobility are some of the acute conditions that can be monitored using RPM technologies.
Patients with The Following Conditions Are Recommended for RPM System.
- At an increased risk of experiencing severe complications
- Having difficulty in attending face-to-face appointments
- Experiencing symptoms for a prolonged period
Each patient’s unique needs are analyzed by a special care team and a strategy is planned.
5 CPT Codes for RPM Reimbursement:
What are the CPT Codes applicable for Remote Patient Monitoring Reimbursement?
In the United States, there are a few different CPT Codes that can be used for remote patient monitoring reimbursement. The most common codes are 99091, 99453, 99454, 99457 and 99458. These codes can be used for a variety of different services, including monitoring vital signs, blood pressure, and blood sugar levels. If you are providing remote patient monitoring services to your patients, you will need to use one of these codes in order to get reimbursed by insurance companies.
So, what are these codes and what do they mean?
CPT Code 99091 is for patient education and self-management support. This code can be used for a variety of services, including providing patients with educational materials, helping them set goals, and providing support to them as they manage their health condition.
CPT Code 99453 is a code used to report Remote Patient Monitoring services. This code can be used to report on a variety of services, including the monitoring of vital signs, weight, blood pressure, and other health metrics. This code can be used by a variety of healthcare providers, including physicians, nurse practitioners, and physician assistants.
CPT Code 99454 is a code used to report the visit of a physician or other qualified health care professional, for the initial care of a new patient. This code is usually used when the physician or other qualified health care professional spends at least 30 (thirty) minutes with the patient.
CPT Code 99457 is for Remote Monitoring of physiologic parameters. This code is used when patients are being monitored for things like heart rate, blood pressure, and respiratory rate. One challenge with CPT code 99457 is that it has always been described at a face-to-face time for 20 (twenty) minutes of continuous time spent providing services.
CPT Code 99458 is for risk reduction interventions and includes counseling patients on health behaviors, medication adherence information, dietary changes, weight loss strategies and referring the patients to other care providers.
These codes are not reported as often as many other non-surgical preventive services codes in primary care. These codes can be billed before or after the patient’s visit to your office, but Medicare requires these services to be initiated by the physician or another designated qualified medical professional within the 7 (seven) days prior to the visit. According to CMS they want PCPs “to proactively use risk mitigation strategies that should incorporate best practices from evidence-based medicine, national guidelines and accepted standards of practice”.
These CPT Codes are used to reimburse physicians and qualified medical practitioners for remote patient care.
Medicare will cover the cost of the equipment, as well as the ongoing management of remote monitoring systems.
CPT 99091 – 30 (thirty) minutes for collection and interpretation of physiologic data.
CPT 99453 – Equipment setup – initial stage and educating patient on the usage.
CPT 99454 – Checking the device’s alert supplies.
CPT 99457 – Minimum 20 (twenty) minutes of treatment and services management and interactive communication with the patient.
CPT 99458 – Physiologic monitoring exceeding 20 (twenty) minutes.
General Requirements for RPM Reimbursements:
1. Patients are imposed with 20% of copayment.
2. Patients are monitored under remote monitoring services for a minimum of 16 (sixteen) days.
3. Skilled physicians or qualified health experts should order RPM services.
4. Synchronized data for evaluation, analysis and treatment.
The new CPT Codes can help to create a healthcare ecosystem that is efficiently accessible, empowered with technologies, standard and affordable. If you are looking at how to utilize CPT Codes for reimbursement and build a better patient care model, MHRCM can help you.
MHRCM are HIPAA complaint revenue cycle management experts who can help to grow the revenues with RPM services

How Can RPM Help Reduce Healthcare Costs?
RPM is a healthcare technology that is becoming increasingly popular in the US. RPM allows doctors and other healthcare providers to remotely monitor their patients’ vital signs and health data. This type of technology has been shown to help reduce healthcare costs by reducing hospitalizations and emergency department visits.
RPM can be used to monitor a variety of different health conditions, including heart failure, diabetes, and asthma. RPM can also be used to monitor patients who have recently been discharged from the hospital. By using RPM, healthcare providers can catch problems early and intervene before they become serious.
There are many different RPM systems in the market, and each one has its own unique features. Some RPM systems allow patients to directly send their health data to their healthcare providers, while others require that the data be sent through a third-party server. Some systems cost more than others, but all of them provide useful health tracking and monitoring capabilities.
The best RPM system for you is likely to depend on your specific needs. If you are interested in a system that can be used by multiple people in your family, an all-inclusive system that includes data storage capacity may be the best option for you. If your focus is on monitoring and tracking a specific aspect of your health, such as blood pressure or weight, you may want to select a system that focuses on one important metric.
What Are Some of the Challenges Associated With RPM?
There are a few challenges associated with RPM that should be noted.
- RPM can be time-consuming, particularly in the initial stages of setting up the system.
- It can be difficult to get accurate data, especially if you are relying on manual data entry.
- RPM can be complex, making it difficult for those who are not comfortable with technology.
Despite these challenges, RPM is a powerful tool that can help you manage your business more effectively. With the right planning and execution, physicians and healthcare centers can overcome these challenges and use RPM to generate Revenue and Reimbursement.
How can Revenue Cycle Management (RCM) Help Reduce the Cost of RPM?
Revenue Cycle Management (RCM) is a process that healthcare organizations use to track and manage patient data from the point of service through to billing and reimbursement.
- RCM can help to reduce the cost of RPM by automating many of the tasks such as Claims Submissions and Denial Management, involved in the billing process.
- RCM can provide visibility into the financial performance of the organization, allowing for proactive decision-making to improve profitability.
Revenue Cycle Management is a process that helps healthcare providers track and manage their patients’ medical billing and payments. This allows providers to optimize their billing and collections process, and ultimately increase their revenues.
What Are the Steps Taken by Healthcare Insurance Providers in Choosing Remote Patient Monitoring?
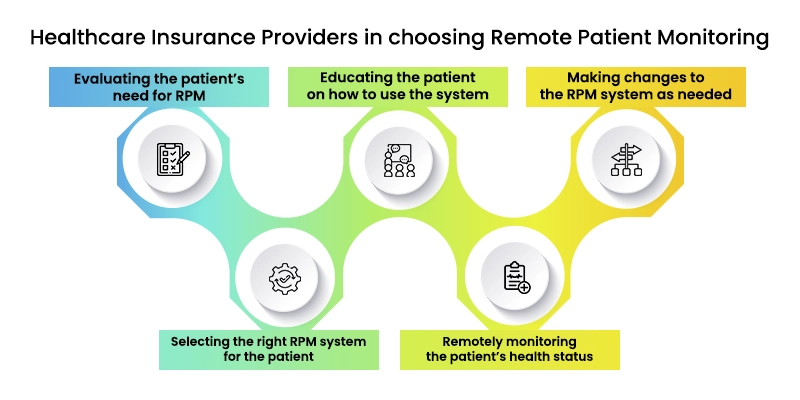
With the advent of new technology, Healthcare Insurance Providers are increasingly turning to Remote Patient Monitoring (RPM) as a way to provide quality care to their patients. RPM is a way of using technology to remotely monitor a patient’s health status, and it has been shown to be effective in reducing the overall costs of healthcare.
When choosing RPM as a way to provide care, healthcare insurance providers will take a number of steps to ensure that the system is effective and safe for their patients. These steps include:
1. Evaluating the patient’s need for RPM
2. Selecting the right RPM system for the patient
3. Educating the patient on how to use the system
4. Remotely monitoring the patient’s health status
5. Making changes to the RPM system as needed
By taking these steps, Healthcare Providers can ensure that their patients are able to receive the best possible care while reducing the risk of hospital readmissions.
How Can You Get Started with Revenue Cycle Management and Remote Patient Monitoring?
There are two main ways that Medical Billing and Coding Companies can help you to reduce the cost of patient monitoring.
- They can help you to get a better understanding of your patients’ medical history and conditions. This will allow you to be able to bill accurately for the services that you provide.
- They can help you to reimburse the costs of monitoring patients. This can help you to limit the amount of money that you spend on patient monitoring.
By reimbursing the cost of patient monitoring, you will be able to reduce the amount of money that is being spent on patient monitoring. As a result, it will be easier for you to stay within your budget. By being able to do this, you will be able to better protect your business from unexpected expenses.
Reimbursement of patient monitoring equipment is an issue that medical practices are aware of. Although there is a body of law governing this subject, many medical practices are not always aware of the specific rules that apply when reimbursing for patient monitoring equipment. To ensure compliance, it is important to understand the different elements that must be included in any claim for reimbursement of patient monitoring equipment.
These Include the Items Listed Below:
- Patient’s name and medical record number.
- Specific dates for which the patient was monitored.
- Reason for monitor use.
- Any co-pay or deductible related to the item(s) being billed.
- Whether the item(s) was / were used by more than one patient during a specific period (for example, if a sleep study machine was used on multiple patients over several days).
- The total amount paid for all items related to the claim (for example, if an overnight sleep study is billed at $400 per night, there would be a total charge of $800 for two studies).
- The total amount paid out by insurance companies or Medicare/Medicaid for all items related to the claim (if a sleep study is paid out through insurance coverage, there would be a total payment made to Medicare or Medicaid).
Wrapping Up:
Despite these challenges, RPM is a powerful tool that can help you manage your business more effectively. With the right planning and execution, physicians and healthcare centers can overcome these challenges and use RPM to generate revenue and reimbursement.
Related Resource :
About the Author