CALL US NOW
(+1) 512 800 6431
(+1) 512 333 4006
MAILING ADDRESS
sales@mhrcm.com
LOCATION ADDRESS
Suite 101, 1250 S A W Grimes Blvd, Round Rock,Texas - 78664, USA
CALL US NOW
(+1) 512 800 6431
(+1) 512 333 4006
MAILING ADDRESS
sales@mhrcm.com
LOCATION ADDRESS
Suite 101, 1250 S A W Grimes Blvd, Round Rock,Texas - 78664, USA
MHRCM, A leader and Expert in Anesthesia Billing & Coding Team.
MedHealth RCM is the complete Revenue Cycle Management and Anesthesia Billing solutions company that streamlines administrative processes and brings remarkable results. We are one of the top Anesthesiology Billing Services in Texas, specialized in Anesthesia Billing and Coding.
As an Anesthesia billing and medical billing services Company Texas, we can understand that each insurance company has different submission requirements. Our Medical Anesthesia Medical Billing Services Team is well-versed with all significant payer regulations.

Our Services
No more errors, no more denials. MHRCM not only proves their excellence in Anesthesia Billing Services and Medical Billing Services, but also submit a well-organized and structured claim in Anesthesiology Medical Billing with the leading Medical Billing Services.
Claim Submission
Our Anesthesiology medical billing specialist team prepares the patient demographics with accurate details and information from step one, to process a clean claim submission for further process.
Claim Follow-Ups
Once we prepare and submit the claims with accurate information, our Anesthesiology billing services specialists proactively follow up with all the claims to verify the status.
Claim Status
We take care to stay on top of all the claims and classify them in a way that makes them accessible and manageable in Anesthesiology billing and coding Services Management.
Payment Posting
Our MHRCM’s Anesthesia billing services and medical billing services Team efficiently does all the Payment Posting for Payments received from the insurance payers via EOB and ERA to track your payment collections.
Improved Revenue
MHRCM’s primary focus is maximizing your Practice’s Revenue. Our Benefits Anesthesia billing solutions makes sure that each Code gets the correct reimbursement quickly and swiftly.
Benefits
Our Full-Suite Denial Management Services for Anesthesiology Medical Billing offer the following benefits for our clients. With Workflow Automation To resolve the Claim’s issue, each Claim Status Code has a set of questions that need to be answered by the Insurance Company. Our A/R Management for effective Accounts Receivable Management in Anesthesiology Billing Services Management, it significantly impacts your Healthcare business’s Revenue and Cash Flow. When successfully completed, it results in Prompt Payments, Satisfied Customers, and High Liquidity for Healthcare.


Clear Anesthesiology Billing Services Management
Transparent & Concise MHRCM Patient Statements
We ensure the Patient Statements are data-driven patient payments, personalized statements requiring industry thinking, and patient-centric research with the registered trademark. Our Anesthesia Billing Services accelerate patient payment with accurate and easy-to-print digital Patient Statements by keeping patient collections faster.
Claim Tracking
We take care of your Denial Claims and are also highly proactive in preventing denials. Our Anesthesiology Billing Services Management constantly focuses on accurate and efficient results. Due to typical challenges and strict Medical Billing Services Regulations, Denial Management became one of the most important pieces of the Healthcare Revenue Cycle Management. Healthcare should focus on the root cause and prevent denials. Denial Management is a time-consuming task and grabs most of the attention on what matters most. Eliminate the challenges and reticulate your time on patient care with MHRCM Denial Management Solutions and Anesthesiology billing solutions.


Precision Billing
Increase your Healthcare Collections by Reducing Staffing Costs with Our Specialized Back-Office Team to maintain the Anesthesia Billing Services and Medical Billing Services from the end-to-end administrative process. Our robust Anesthesia Billing solutions are proven to minimize your errors and denials to get paid faster.
General Manager, Empower Therapy
VP, Finance, Quartz Health

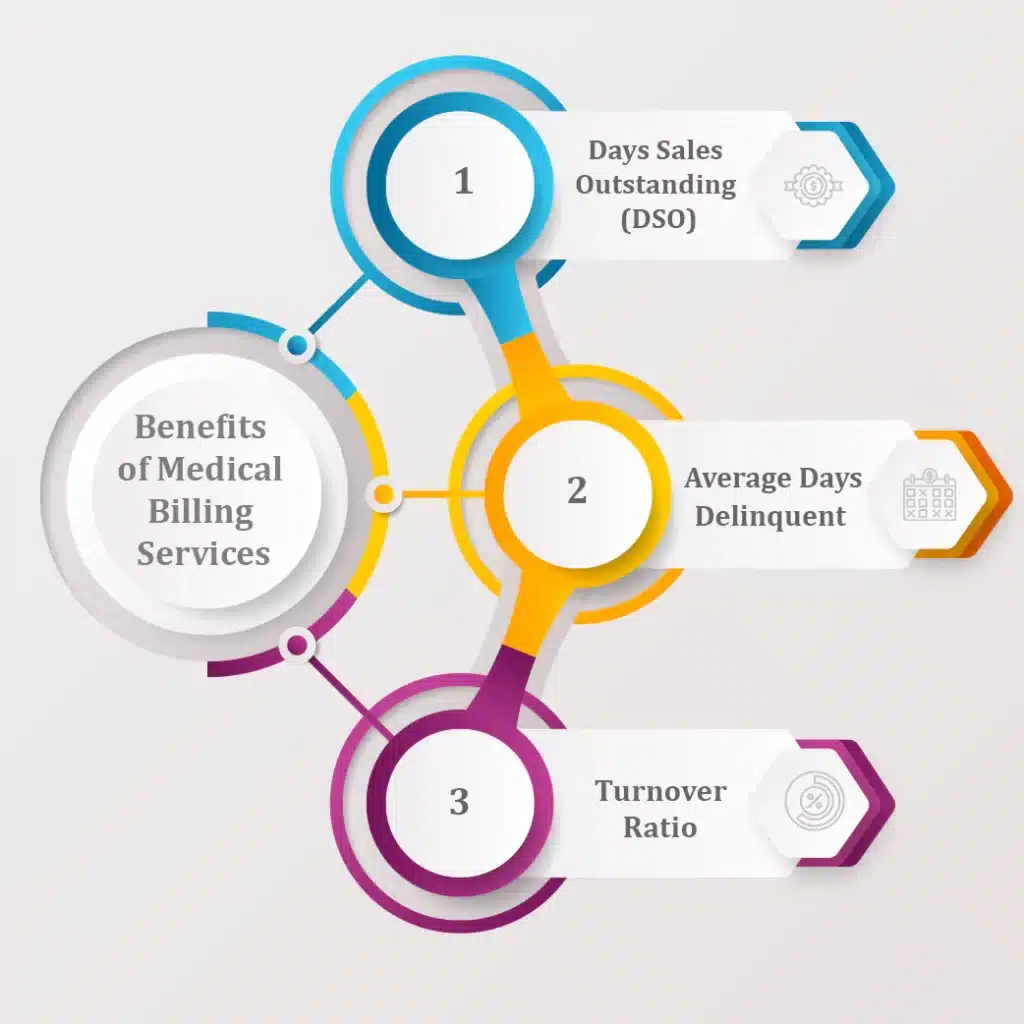
Average Days Delinquent is another important factor that should be kept low, and our Anesthesiology Medical Billing Back Office Team strives to maintain it for you. It is the number of days on average that a client Payment is Overdue. We ensure that by maintaining a flawless Anesthesia CPT Codes, Medical Billing Services and AR Management.
Frequently Asked Questions
Copyright © 2026 MHRCM All rights reserved. Designed By InfinityHub