Mental health comprises our emotional, psychological, and social well-being. It is how we think, feel and behave. It also helps determine how we handle stress, relate to others, and make choices.
Behavioral disorders are a type of mental health disorder that is characterized by abnormal patterns of behavior. These disorders can significantly interfere with a person’s ability to function in daily life. Some common examples of behavioral disorders include ADHD, OCD, and autism.
Mental illness is one of the most common conditions in the United States, affecting tens of millions of people each year. Though mental illness is highly treatable, many people do not seek or receive treatment due to cost, lack of access, or stigma.
Medical insurance is a critical tool for ensuring that people with mental illness can get the treatment they need. In recent years, however, insurance companies have been increasingly reluctant to cover mental health services. This has led to a rise in the number of people who are unable to afford treatment.
Mental health billing is a complex and ever-changing process, and it can be difficult for service providers to keep up with the latest changes. As a result, many providers are at risk of being underpaid or not paid at all for their services. This can lead to financial problems for providers and, in some cases, to the closure of their practices. When it comes to billing for behavioral disorders, the process can be even more challenging. There are a number of different codes used to bill for these types of disorders, and it is a little difficult to know which one to use in each case.
In addition, there are a number of different factors that can affect the cost of treatment for these disorders. This can make it difficult to estimate the cost of care in advance.
Mental Health Billing is so difficult for healthcare organizations because of a number of reasons.
1. There are many types of insurance plans and each one has its own set of rules and regulations. This makes it difficult to know how to properly submit claims and get reimbursed in a timely manner.
2. The Second challenge is that many insurance companies require pre-authorization for certain types of services. Healthcare organizations need to obtain approval from the insurance company before providing certain types of services to their patients. This is a time-consuming process and delays service reimbursement.
3. Most insurance plans only reimburse a portion of the total service cost to mental health services. It often ends up footing a substantial amount of the patient’s bill in order to ensure that they receive complete care.
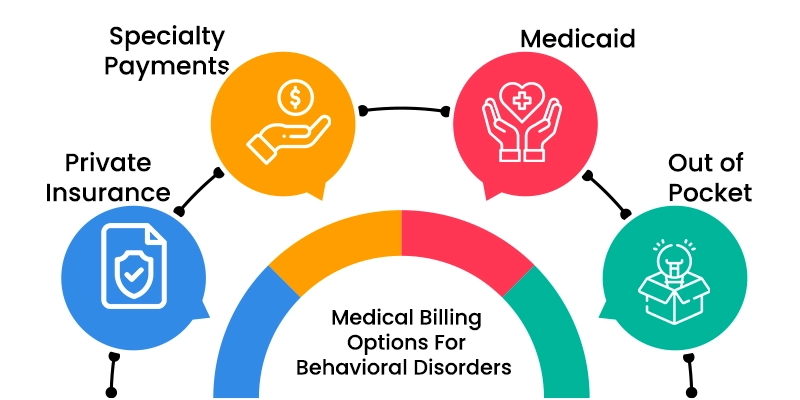
There are a few different medical billing options for behavioral disorders. The most common ones are:
Specialty Payments: You can receive specialty payments for treating behavioral disorders. This type of payment is usually higher than the standard payments that you would receive for other types of care.
Medicaid: You can bill Medicaid for behavioral disorders. Medicaid is a government program that provides health insurance for low-income people.
Private Insurance: You can bill private insurance companies for behavioral disorders. Private insurance companies typically have higher reimbursement rates than Medicaid.
Out-of-Pocket: You can also choose to bill patients out-of-pocket for their treatment. This option is usually only viable if you have a small number of patients.
Larger health groups face unprecedented challenges in medical billing process. Behavioral health centers are not an exception. They also face difficulties due to denials in medical bills and complex payment methods of insurance companies. Behavioral health patients are opting for self-pay due to the more complex RCM systems. Some healthcare providers feel that unique rules, guidelines and requirements set by insurance service providers makes them difficult to get reimbursements.
Behavioral health services have only two options in RCM. Inhouse billing and Outsourcing.
Managing RCM in-house is possible with expert staffs and resources in hand. A strong EHR billing system specific for Behavioral Health Sciences minimizes the risk of human error. If healthcare service provider lacks in any of this, then outsourcing the medical billing process is the best choice.
Outsourcing Medical Billing Service:
Outsourcing medical billing services to medical billing companies is always considered the best option because they have all the tools and software needed for efficient medical billing services. Most medical billing companies provide 24/7 customer support and they reduce the burden of recruiting and maintaining a talented team of medical billing and coding.
Here are some suggestions to assist mental health practitioners effectively and efficiently in billing for the services they provide, resulting in fewer denials, more money for the company, and more time for helping patients.
1. Check the insurance of each patient’s coverage and benefits prior to the delivery of service.
2. Get pre-authorization or utilize in-network providers, when possible, to avoid issues with billing later on.
3. Be well-versed in codes for specific diagnoses and services so that you can correctly bill for them.
4. Submit claims as soon as possible after service delivery to avoid any delays in reimbursement.
5. Keep accurate and up-to-date records of all patient encounters, including dates, diagnoses, services rendered, and insurance information.
6. Follow up with insurance companies regarding claims that have been denied or are taking a long time to process.
7. Be familiar with the appeals process in case a claim is denied and you need to file an appeal.
8. Consider using billing software or hiring a billing company to handle claims submission and follow-up so that you can focus on patient care.
As the behavioral health industry continues to grow, more and more practices are considering outsourcing their Revenue Cycle Management (RCM) services. RCM is a vital part of any healthcare practice, but it can be time-consuming and complex. By outsourcing your RCM services, you can focus on your patients while leaving the billing and collections to a team of experts
There are many benefits of outsourcing your RCM, but here are a few of the most important:
Access to the Latest Technology and Tools: While outsourcing RCM, you can access the latest technology and tools of the service provider. Access to the latest technologies helps to streamline the billing and collection process and makes it more effective and efficient.
Save Time and Money: Outsourcing RCM can save time and money. By outsourcing billing and collections, you’ll free up staff to focus on other areas of your practice. This can lead to increased efficiency and productivity and ultimately saves money.
Improves Patient Satisfaction: Outsourcing RCM can improve patient satisfaction. Patients receive their bills quickly and easily and have less worry about contacting the healthcare provider’s office to make payments.
Increase Cash Flow: One of the biggest benefits of outsourcing RCM is that it can increase the cash flow. By outsourcing billing and collections, you can receive payments more quickly, which will ultimately lead to more money.
Behavioral health organizations, like all other medical practices, must be able to bill for their services in order to receive compensation. However, the billing process for behavioral healthcare is complex, as Insurance providers need to track different types of services and diagnoses. This is where medical billing software can be beneficial.
Medical Billing Software assists practices in handling payments, managing claims, and increasing revenue more efficiently than using a typical billing program. It streamlines the collections and billing processes and therefore the revenue cycle gets faster and improves the overall profitability. RCM software bridges the gap between electronic health record, also known as EHR programs and the accounting system.
How to Select a Medical Billing Software for Behavioral Health Services?
Medical billing for behavioral health practices can be a complex and time-consuming process. There are many different diagnosis codes, treatment codes, and insurance coverage considerations that need to be taken into account. In addition, it is important to keep up with the ever-changing rules and regulations regarding reimbursement from insurance companies.
One way to streamline the medical billing process is to use a comprehensive medical billing software solution. Billing software can automate many of the tasks associated with medical billing, including claims processing, claims management, and Accounts Receivable (A/R) follow-up. In addition, medical billing software can help you keep track of your financial data, providing valuable insights into your business operations.
When selecting a medical billing software solution, it is important to choose one that is designed specifically for behavioral health practices. Apart from the insurance claims, they have features such as:
Psychotherapy Notes – Documentation tools that capture each patient interaction in an easily accessible format. This information can be used for clinical decision-making, treatment planning, and progress reports.
Medication Management – Providers can record medication prescriptions and refills, as well as staff updates on medication adherence. These tools also reduce duplicate charting for patients who receive prescribing from both a physician and behavioral health provider.
Assessment Tools – Assessment forms or screening tools that provide the patient profile are often used in treatment planning.
Integrated Clinical Documentation – digitized clinical documentation and picture archiving & communications systems allow your practice to replace paper charts with electronic records, improving communication between care providers and enhancing the security of sensitive information. It significantly improves the reimbursement rate.
As a behavioral health specialist, you provide your patients with critical and sensitive services. Because of this, it’s imperative that you select the right billing company to partner with. A bad or inexperienced provider can not only frustrate your patients but also put your reputation at risk. If you currently have an assistant or team member who handles your billing operations, you might be hesitant to outsource those responsibilities. After all, if something goes wrong, it could reflect poorly on you and your practice as a whole. However, by considering the benefits of different billing options for behavioral health specialists, you can easily reduce stressors and ensure that both you and your team are operating as efficiently as possible — so that you can focus on what really matters: patient care.