Billing is a fundamental aspect of the healthcare industry. Accurate and efficient billing ensures that healthcare providers receive timely payments for their services, maintain financial stability, and continue to offer quality care to patients. In this article, we will explore the specific differences between Mental Health Billing and Medical Billing, shedding light on the unique aspects that set them apart.
Key Differences Between Mental Health Billing Services and Medical Billing Services
1. Patient Diagnoses and Treatment Codes
One of the primary distinctions between Mental Health Billing and Medical Billing lies in the Patient Diagnoses and Treatment Codes used. Mental Health Diagnoses and Treatment Codes differ significantly from those found in Medical Billing. Mental Health Practitioners rely on diagnostic criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) to classify patients’ conditions accurately.
Accuracy in code selection is crucial in Psychiatry Medical Billing, as it directly impacts Claims Processing and Reimbursement. Mental Health Practitioners must be well-versed in the DSM-5 and other relevant coding systems to ensure proper documentation and coding for their services.
Insurance Coverage for Mental Health Services varies from Medical Services in several ways. Different insurance plans may have distinct coverage policies, copayments, and deductibles for mental health treatments. This variation often stems from historical stigmas associated with mental health, but it’s worth noting that regulations have been put in place to address these disparities.
The Mental Health Parity and Addiction Equity Act (MHPAEA) is a federal law that mandates equal insurance coverage for Mental Health and Medical Services. This law ensures that insurance providers cannot impose more restrictive limitations on Mental Health Coverage compared to Medical Coverage. Despite these legal protections, disparities in insurance coverage may still exist based on individual insurance plans.
3. Documentation and Compliance
Mental Health Billing and Credentialing Services also differs significantly when it comes to Documentation and Compliance requirements. Mental Health Practitioners must maintain meticulous records, including progress notes, treatment plans, and informed consent documentation. These records are essential for tracking a patient’s progress, ensuring continuity of care, and substantiating the need for services.
However, Mental Health Billing poses unique compliance challenges, particularly concerning patient confidentiality. Practitioners must adhere to strict HIPAA regulations to safeguard patients’ sensitive information. Failure to comply with these regulations can lead to severe consequences, including legal and financial penalties.
By recognizing the disparities in Patient Diagnoses and Treatment Codes, Insurance Coverage, and Documentation and Compliance, Healthcare Professionals can navigate the complexities of Mental Health Billing more effectively and provide quality services to those in need.
Reimbursement Rates are a critical consideration in both Mental Health Billing Services and Medical Billing Services.
Mental Health Reimbursement Rates can vary widely based on several factors, including the Specific Insurance Plan, Geographic Location, and the Type of Mental Health Service provided. Generally, Mental Health Services may have lower Reimbursement Rates compared to Medical Services. This discrepancy has historical roots in the way mental health has been historically perceived and prioritized within the healthcare system.
However, it’s important to note that efforts have been made to address this disparity. The Mental Health Parity and Addiction Equity Act (MHPAEA) aims to ensure that Mental Health and Medical Services receive equal reimbursement treatment from insurance companies. Despite this legislation, challenges related to Reimbursement Rates persist, and Mental Health Practitioners often need to advocate for fair compensation.
5. Billing Software and Systems
The field of Mental Health Billing relies on specialized Billing Software and Systems designed to meet the unique needs of Mental Health Practices. Mental Health Billing Software is designed to accommodate the specific diagnostic codes (such as those from the DSM-5) and the intricacies of Mental Health Service Billing. It should also be capable of handling different insurance requirements, including Preauthorization and Claims Submission.
Patient Information Management: Keeping detailed patient records and demographics.
Appointment Scheduling: Managing appointments and keeping track of billing for each session.
Electronic Claims Submission: Simplifying the process of submitting claims to insurance providers.
Coding Assistance: Providing guidance on appropriate Diagnostic and Procedural Codes.
Reports and Analytics: Offering insights into billing performance and revenue trends.
Choosing the right Billing Software like MHRCM is crucial for Mental Health Practices to ensure Efficient Billing Processes and Compliance with Regulations.
6. Staff Training and Expertise
Effective Mental Health Billing relies on trained staff with expertise in the unique aspects of Mental Health Billing Services
Mental Health Billing requires a deep understanding of Mental Health Diagnostic Criteria, Treatment Codes, Insurance Coverage Nuances, and Privacy Regulations. Staff members responsible for Billing should undergo specialized training to navigate these complexities effectively.
Training Should Encompass:
Understanding Mental Health Diagnoses: Staff should be proficient in the DSM-5 and other relevant diagnostic tools.
Insurance Knowledge: Familiarity with different Insurance Plans and their Mental Health Coverage Policies is essential.
HIPAA Compliance: Training on maintaining patient confidentiality and adhering to privacy regulations.
Billing Software Proficiency: Staff should be skilled in using Specialized Billing Software and Systems.
Hiring or training staff with expertise in Mental Health Billing ensures accurate claims submission, reduces errors, and enhances the practice’s overall financial health.
Overcoming Challenges in Mental Health Billing
Dealing with Billing Denials and Appeals is a common challenge in Mental Health Billing. Billing Denials can occur for various reasons, such as incomplete documentation, coding errors, or insurance-related issues. To overcome Denials, Mental Health Practices should have robust processes in place to review claims before submission, ensuring accuracy and completeness. When Denials do occur, prompt action is essential.
Strategies for handling Denials and Appeals include:
Thorough Documentation: Maintain detailed records to substantiate the necessity of services.
Review and Correction: Analyze Denials, identify the root causes, and correct errors promptly.
Appeal Process: Develop a structured approach to Appeal Denied Claims, providing additional information and documentation as needed.
Communication: Establish open lines of Communication with Insurance Companies to resolve issues efficiently.
Effectively managing Denials and Appeals is crucial for ensuring that Mental Health Practices receive the reimbursement they deserve.
Privacy and Confidentiality
Addressing Privacy and Confidentiality concerns is paramount in Mental Health Billing.
Mental Health Practitioners handle highly sensitive patient information, including diagnoses, treatment plans, and progress notes. Maintaining Patient Confidentiality is not only an ethical obligation but also a legal requirement under HIPAA.
To ensure Privacy and Confidentiality in Mental Health Billing:
Access Control: Restrict access to patient records to authorized personnel only.
Data Encryption: Secure electronic records with strong encryption to prevent unauthorized access.
Secure Communication: Use secure channels for transmitting Patient Information and Billing Data.
HIPAA Compliance: Stay updated with HIPAA regulations and implement necessary safeguards.
Failure to protect Patient Confidentiality can result in severe legal and ethical consequences, making it imperative for Mental Health Practices to prioritize privacy.
Communication with Patients
Effective Communication with Mental Health Patients regarding Billing and Payments is vital. Billing discussions in Mental Health Practices can be sensitive, as patients may already be dealing with emotional and psychological challenges. To ensure a positive patient experience:
Transparency: Be transparent about Billing Practices, Insurance Coverage, and any Out-of-pocket Costs.
Education: Provide patients with information about their rights and responsibilities regarding Billing.
Payment Options: Offer flexible Payment Options to accommodate patients’ financial situations.
Billing Inquiries: Establish a clear process for addressing Patient Billing Inquiries and Concerns.
Empathy: Approach Billing conversations with Empathy and understanding of patients’ emotional states.
Effective Communication can enhance patient trust and satisfaction while reducing misunderstandings and conflicts related to Billing.
Best Practices for Mental Health Billing
Stay Informed About Regulations
The Healthcare Industry is subject to constant regulatory changes, and Mental Health Billing is no exception. To maintain compliance and maximize revenue, Mental Health Practices must stay updated with evolving regulations at the federal, state, and local levels.
Best Practices for Staying Informed About Regulations include:
Continuing Education: Attend seminars, workshops, and webinars focused on Mental Health Billing Regulations.
Professional Associations: Join Associations related to Mental Health Billing to access resources and updates.
Consultation: Consider seeking legal or compliance experts’ guidance to ensure adherence to regulations.
Proactive compliance with regulations not only minimizes risks but also contributes to a smooth and ethical Billing process.
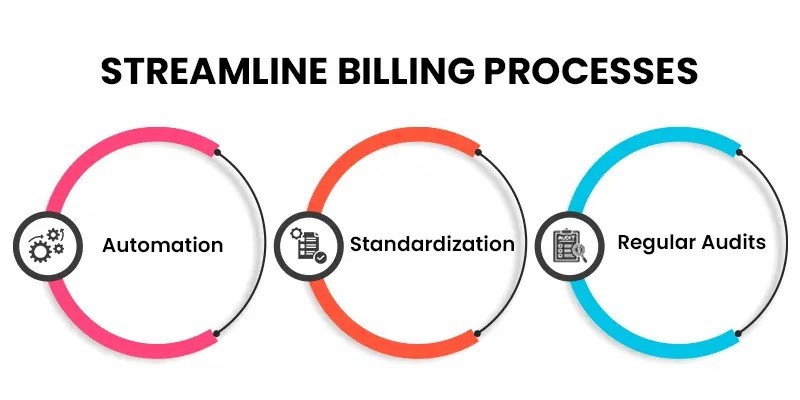
Streamline Billing Processes
Efficiency is key in Mental Health Billing Services. Streamlining Billing Processes can reduce administrative burden, minimize errors, and expedite reimbursement. Strategies for achieving this include:
Automation: Implement Billing Software features that automate repetitive tasks.
Standardization: Develop Standardized Billing Procedures and Documentation Templates.
Regular Audits: Conduct Regular Audits to identify and rectify Billing inefficiencies.
Training: Continuously train staff on efficient Billing Practices.
Efficient Billing Processes contribute to a healthier bottom line and allow Mental Health Practitioners to focus more on patient care.
Outsourcing Mental Health Billing to Professional Billing Services can offer numerous advantages.
Outsourcing Mental Health Billing can free up valuable time and resources for Mental Health Practitioners. Professional Billing Services are equipped with the expertise, software, and infrastructure to handle Mental Health Billing effectively. They can:
Maximize Revenue: Billing experts are adept at Optimizing Reimbursement Rates and Reducing Denials.
Ensure Compliance: Professional services stay current with regulations to maintain Compliance.
Reduce Administrative Burden: Mental Health Practitioners can focus on patient care while professionals handle Billing tasks.
While there are costs associated with outsourcing, many practices find that the benefits outweigh the expenses, ultimately leading to improved financial health and peace of mind.