Medical Billing is the process of creating healthcare claims to submit to insurance companies to receive reimbursement for medical services provided by providers and provider groups.
The biller tracks the claim after converting a healthcare service into a bill. A skilled medical biller helps to improve the revenue performance of a healthcare service provider.
The Medical Billing service consists of multiple processes. The process might take anywhere from a few days to several months. The goal here is accurate billing and quick follow-up. In most cases, insurance companies are required to pay claims within 30 or 45 days. The late claim might be refused without the opportunity to appeal, and the organization is not reimbursed in that case.
Medical Billing service needs more effort and practice, as errors at any stage of the billing cycle can be expensive in terms of income and administrative effort. The performance of the front-end and back-end billing personnel involved here is critical to the financial health of medical practices and healthcare providers.
The Revenue Cycle Management process involves a series of processes to ensure a smooth payment process.
The personal data of the patient is not the complete record that Medical Revenue Cycle Management services require. It needs the medical data of the incident. The medical biller collects data from the physician about the patient’s diagnosis for insurance purposes
The medical service provided for the patient is recorded along with the service charge. This data helps the Revenue Cycle Management process identify and determine the associated insurance costs.
To maintain a consistent and accurate insurance plan, the Revenue Cycle Management healthcare system needs to collect and maintain all this data for individual patients. The Medical Billing service really starts here!
Medical Billers’ actual responsibility starts with negotiating the reimbursement for healthcare services with individuals, healthcare providers, and insurance companies. The reimbursement negotiations are based off the collected patient data and insurance history. This data is verified by the Medical Biller before submitting for the claim.
The Medical Billing process can be divided into front-end and back-end process. Front end billing process refers to services prior to service—that is, before the service is provided to the patient. In this process, a front-end billing personal maintains all the data and information of the patient.
Front-end Medical Billing in Revenue Cycle Management strategy requires a professional practice. The biller who’s familiar with the organization’s insurance payers and health plans. They must be a trained billers to identify insurance eligibility while also remaining aware of filing deadlines.
The Revenue Cycle Management process for processing an insurance claim begins when the patient registers for an appointment with the doctor. After the registration, the data collection process begins. Here, a Medical Revenue Cycle Management service provider needs to follow a standard procedure to maintain an accurate database.
Eligibility Verification involves a verification of patient’s insurance eligibility such as the dates, patient coinsurance, copay, deductible, and plan benefits.
The patient is now informed about the financial details after the verification of insurance claim eligibility.
The front-end staff schedules follow-up appointments as needed and ensures that the insurance form is updated. Medical coders obtain the patient’s medical records and convert the billable information into medical codes after the patient has checked out.
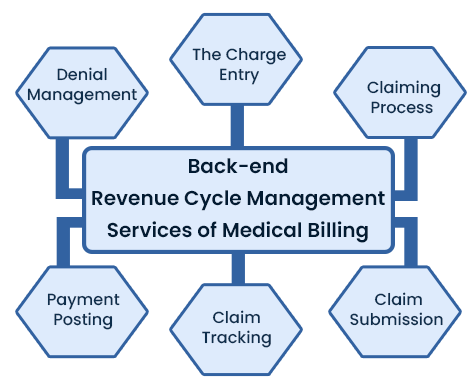
The back-end process of Revenue Cycle Management involves various stages and documentation to ensure the revenue flow is maintained.
In Revenue Cycle Management solutions, Charge Entry refers to the process of calculating the amount of reimbursement that the provider will receive from the insurance payer.
After finalizing the charges and payments, the claiming process is initiated. The Revenue Cycle Management service process claiming is based on the data derived from the bill generated.
Bill claims are submitted through clearinghouses, which provide a variety of services, including the review of claims for compliance with payer policies and federal regulations. The clearinghouse will return claims that require corrections to the biller before forwarding the corrected claims to the payer.
When the claim reaches the payer after passing through the clearinghouse, the data file is processed and converted to a claim form for the claims revie
.
Claim-submitted bills must be inspected on a daily basis. When a claim reaches the payer, adjudication begins. Adjudication refers to the process of reviewing a claim and determining whether or not a payer will pay the provider. So, this should be tracked.
Payments must be posted on the day the physician starts the practice, along with accompanying checks or direct deposits. The Revenue Cycle Management service provider must verify that the billing matches payments to patient accounts, reconcile payments against claims, and confirm the data. Finally, Medical Billers must reconcile direct deposits received and posted.
When an insurance provider denies a claim, the remittance advice includes a denial code with a brief explanation. The billing staff should review the denied claim to determine if additional information is required, if errors need to be corrected, or if the denial should be appealed.
We are clear on all the processes and procedures of Medical Billing services. If you ask whether you can handle the Revenue Cycle Management billing process in-house, then here’s few points to consider.
Outsourcing your hospital’s Revenue Cycle Management entails bringing in an outside team to handle all of your administrative tasks related to billing, coding, and other non-provider-related tasks. This allows your entire team to concentrate on helping people rather than worrying about how to maintain the Revenue Cycle Management process.
Outsourcing your Revenue Cycle Management should reduce Medical Billing and Coding errors while also streamlining patient and insurance provider collections. This will help to ensure that all of those funds that were pending have been collected completely.
You no longer need to invest time in hiring, training, and managing billing staff if you outsource RCM. Outsourcing RCM allows you to devote more time to making the most of your medical expertise, improving patient care, and expanding your practice.
Furthermore, the outsourcing of Revenue Cycle Management services can cover all possible revenue generation process for your company. They will handle everything, from negotiating with insurance companies to following up for delayed payments to disputing claim denials.