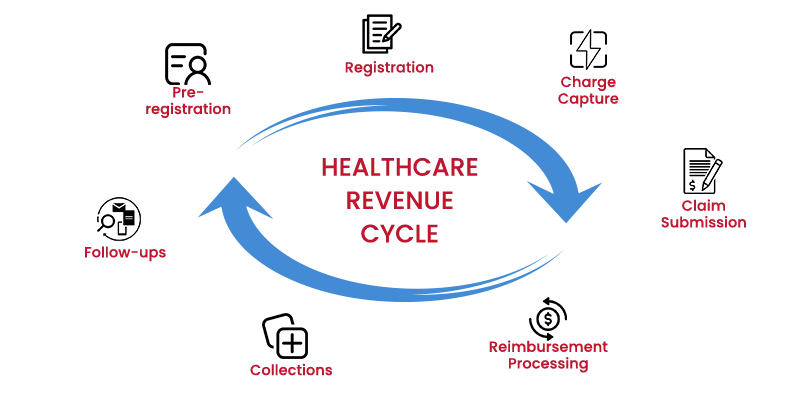
The healthcare revenue cycle includes all the administrative and financial processes involved in the capture, management, and collection of patient service bills. It is the process of tracking and analysing the patient’s revenue, right from their registration to final payment collection.
Revenue Cycle Management, like accounting, considers certain factors to determine the process. It includes the cost of a care facility to the patient. We can even identify the procedure or methods of a suitable care facility for a patient, that generates the most revenue.
With Revenue Cycle Management solutions, once all the required information is obtained, administrators at a care facility can determine where funds should be allocated and how to boost income to fund a broader range of services to satisfy patient requirements.
An effective Revenue Cycle Management strategy assures accurate Billing and timely Reimbursement while reducing rejections. It involves a wide range of stakeholders, including healthcare professionals, insurance companies, and patients in the cycle.
Implementing an effective Revenue Cycle Management process is important for healthcare providers to maintain financial stability while providing exceptional patient care. A well-managed medical revenue cycle allows healthcare businesses to optimize cash flows, manage operating expenses, and deploy resources more efficiently.
Improved Revenue Cycle Management enables precise financial forecasting and budgeting, allowing healthcare organizations to make precise decisions on investment, expansion, and strategic collaborations.
Increased cash flow is one of the primary benefits of effective Revenue Cycle Management. By implementing efficient Billing and Collection processes, healthcare providers can reduce the time it takes to receive payments for services. It improves the organization’s financial stability and ensures that necessary funds are available to provide quality patient care.
Healthcare professionals often face crises where they need to provide more attention to patients, rather than other operational activities. When there’s a pandemic crisis, the healthcare system has more emergency situations to handle, and there are a number of issues that require immediate attention and action. This stressed the importance of implementing an effective Revenue Cycle Management process in many healthcare firms.
With the cancellation of non-essential treatments and the drop in patient loads during the epidemic, hospitals and health systems have faced substantial financial strain.
The loss of revenue from these sources has underlined the importance of Healthcare Revenue Cycle Management strategies that can adjust to changing conditions.
Healthcare providers can acquire significant insights into patient demographics, care trends, and reimbursement patterns by employing data analytics in their systems. These insights help them identify possibilities to better utilize capacity, maximize outreach efforts, and adapt community offerings.
This information is sent to the patient’s insurance provider and then to the provider’s Practice Management System, which informs the healthcare about the patient’s coverage, deductible, co-insurance, co-payment, and a referral if required.
Patient’s financial expectations, time of the payment and cancellation policies are decided during this stage.
Registration process is to verify that all the patient’s information is correct from beginning to end. The Revenue Cycle Management service provider ensures that the patient’s address, phone number, date of birth, guarantors, and insurance information are correct during registration.
The provider collects co-payments during registration, and a specialist will confirm that a referral or authorization is needed for a patient. Financial paperwork is signed, and insurance benefits are assigned during registration. If these processes are not followed and the practice is audited, there is a possibility of financial repercussions.
Both approaches have advantages and disadvantages, as there are charges that can be missed either way.
An expert auditor can trace a charge from start to end as part of a Revenue Cycle Audit to detect missing charges and identify fraud.
The Revenue Cycle Team should investigate the charges, CPT codes, and diagnostic codes and inquire whether the diagnostic will support the procedure. If two services are given, they must be separated and suitably coded. Claim Submission is the process of ensuring that claims are fair and properly processed. If a claim is accurately submitted to the insurance carrier, it will be paid much sooner.
After a claim has been processed, Reimbursement Processing begins. The benefit explanation shows how much they were paid for the services offered. Allowables agreed upon are determined during this phase.
A mistake that can happen during this phase is “post and go”. When a claim is submitted and forgotten, that is, if the carrier does not pay or something is configured wrong in the Practice Management System, the problem may be overlooked in the “post and go” scenario.
Patient Collections is the most problematic aspect of the Revenue Cycle procedure. It is suggested that front desk personnel collect at the time of service. To keep the collection growing, make sure you have a uniform policy in place for collecting copayments and deductibles that establishes the practice’s financial expectations. It is equally crucial to ensure that routine patient statements are distributed. A daily statement cycle is a best practice.
Your patients will receive one statement every 30 days, but statements will be sent out more often, allowing you to move your revenue cycle more swiftly and expedite your cash flow. Cleaning up your patient collections will help you avoid hiring a bill collector.
Healthcare Revenue Cycle Management continues to grow and adapt to its rapid changes, such as value-based care, technology development, and a worldwide pandemic. In order to offer adequate treatment to patients and get correct reimbursement for services, healthcare personnel should always be informed of their revenue cycle status.
A custom Revenue Cycle Management service provider team like MHRCM, is needed to consolidate all of the reports you require, into a single location for real-time access.
These seven revenue cycle processes provide a comprehensive overview of how MHRCM will assist your healthcare programs with effective RCM service. Healthcare providers can benefit from increased operational efficiency and timely revenue management by improving accuracy and streamlining operations. If you’d like to learn more about how we can assist you with managing your revenue cycle, connect with our experts today!
Frequently Asked Questions: