RCM’s collection in medical billing plays a key role because the medical claims assessors will review each claim and issue payment. If they find any problems with it, they will return it with a reason why they are in denial. The medical officer is responsible for correcting the problem and making corrections.
Why is it Important to Improve the Collection Process?
Challenges in the Collection Process:
Many healthcare centers and practices are still struggling to increase practice revenue and patient volume. Though the pandemic has crossed its border, there is still a heavy decline in patient visits to surgical specialties and pediatric practices.
One of the best ways to increase the practice revenue is by increasing the patient collection process. This in turn will help you maintain the cash flow.
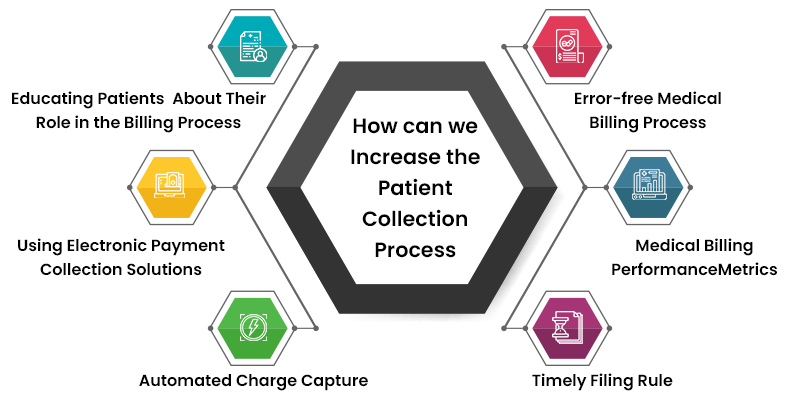
But How can we Increase the Patient Collection Process?
Improving the patient collection process in any healthcare provider cannot happen in a single day; a clear and consistent plan is required for a steady cash flow.
In this blog, MHRCM shares some tips to increase the patient collection process.
Educating patients about their role in the entire billing process is important to increasing medical billing collections. Patients need to understand that a percentage of their payments are due at the time of service. In addition, patients need to be aware of available payment options, such as electronic and digital processing. In addition, patients need to understand that they are responsible for their bills. By educating patients about these issues, healthcare providers can improve the overall experience for patients and increase payment collections.
Using Electronic Payment Collection Solutions
Regardless of whether you accept cash, credit cards, or check payments, using electronic payment collection solutions can help you increase your medical billing collections. By using a reliable payment collection solution, you can reduce the number of bills sent to collections, simplify cash flow, and reduce the amount of time and resources needed to investigate and resolve incorrect or missed invoices. Your patients deserve the same service, so make sure they understand the costs upfront. Providing an online account allows patients to pay online, reducing the time and money spent on collection calls.
Several advantages of using electronic payment collection solutions include reducing bad debt and reducing account receivable days. In fact, according to a recent survey, 20% of providers say that implementing a credit card on file program is the best solution for reducing accounts receivable days. Additionally, the use of a credit card on file program has been shown to reduce write-offs and bad debt. Survey results show that patients prefer electronic payment collection solutions when the amount of the bill is less than $200.
When implemented correctly, automated charge capture for medical billing collection in Revenue Cycle Management can significantly improve the revenue cycle for a provider. Charge capture is the process of entering patient information, such as name, address, and a description of care, into a system that transforms the data into a claim, which is submitted to the insurance company for reimbursement. The key benefits of automated charge capture include a reduction in keystroke errors and reduced time spent entering data manually.
In RCM, timely filing is a crucial step to revenue capture. The goal is to submit a claim within a payer-defined deadline. For example, a 90-day deadline means that a claim must be submitted within ninety days of service. While this seems simple enough, it can be difficult to determine which payers require a 90-day timeframe. To help you understand your payer’s requirements, check your policy manual or check out some online resources.
Medical Billing Performance Metrics
Error-
Free Medical Billing Process:
Nearly 80% of all medical claims contain errors. Error-prone claims have a longer claim cycle, which can reduce collections. Incorrect information and double-checking claims will reduce the amount of claims that are rejected by insurance carriers. They can also help your practice scale its operations. And finally, medical billing services can ensure your systems are robust enough to withstand the inevitable rise in patient volume.
Communicating with Health Insurance Companies
Successful communication with health insurance companies is critical for revenue capture. A good billing team understands the requirements and coding of each insurance company, explains why a claim was denied, and appeals claims that are not paid. With nearly 4 percent of claims being denied on the first try, it is crucial that the billing team understands why a claim was denied. It is also vital that the team understands the patient’s deductibles and co-pays, and that they are communicating payment plans.
Communication with health insurers is important to maximize medical billing collections from patients. Before a patient visits, staff members will verify insurance coverage and collect the patient’s copayment. A medical coder will then categorize the patient’s visit based on ICD-10 codes. Insurance companies will pay part of the fee, with the remainder paid by the patient. Managing claims with proactive claims management is critical to improving the net collection ratio, decreasing days in accounts receivable, and increasing per-encounter reimbursement.
Outsourcing Medical Billing
Medical billing outsourcing has several benefits. Outsourcing medical billing reduces the risk of common medical billing errors. Outsourced teams can avoid data entry errors, duplicate billing, inaccurate demographics, and upcoding. They can stay up to date with ever-changing billing regulations. The team will also appeal denied claims. An experienced company will send appeals with all of the relevant information. Outsourced teams are more efficient than in-house billing departments
In-house billing is typically handled by administrative staff hired by medical practices. Although these employees are often highly trained, they are not always up to date on new laws and regulations. The risk of failure to stay compliant is high when a practice doesn’t regularly provide staff training. However, outsourced medical billing companies have a dedicated billing section that will provide training and keep up with the latest regulations. In addition to their knowledge and experience, they are also trained regularly by an experienced team.