Are you a medical practice or healthcare facility looking to switch your medical billing software? Making a software transition can be intimidating, especially when it comes to something as crucial as managing your revenue. MHRCM guides you through the process of switching medical billing software without any negative impact on the revenue.
How to Switch Medical Billing Software without Affecting Revenue?
1. Assess Your Current Software:
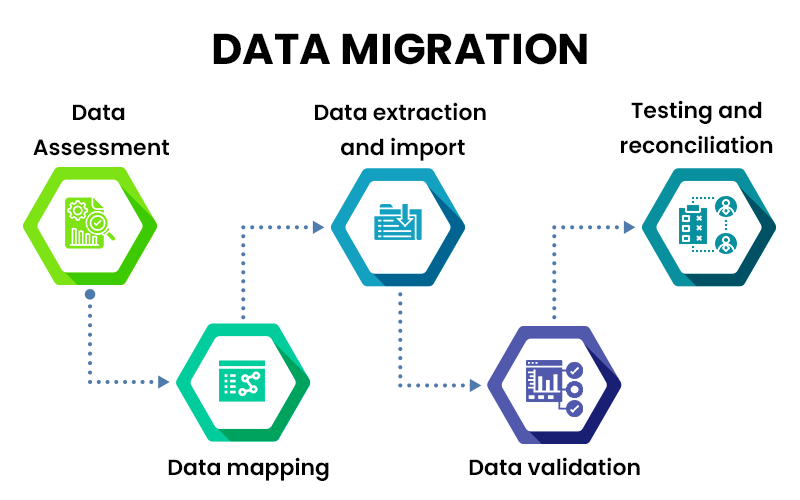
6. Data Migration:
One of the critical aspects of switching Outsource medical billing service is the seamless migration of your data. As you transition to the new software, you must ensure that all your existing patient, billing, and financial data is accurately transferred. Data migration can be a complex process, so working closely with your new software provider to facilitate a smooth transition is essential.
Parallel Running offers Several Benefits
9. Monitor and Address Issues:
During and after the transition to the new medical billing software, it is crucial to closely monitor its performance and promptly address any issues. Pay attention to the revenue stream, coding accuracy, claims submissions, and payment cycles to ensure the software does not negatively impact your revenue.
10. Continual Support and Upgrades:
- Consultants
- Industry Associations
- Software Vendor Support





