What Is Anesthesia Billing and Revenue Cycle Management (RCM)?
Medical billing for anesthesia can turn into a convoluted process, as it requires reporting a few records, including:
- Pre-operative review
- Anesthesia sheet
- Post-operative review
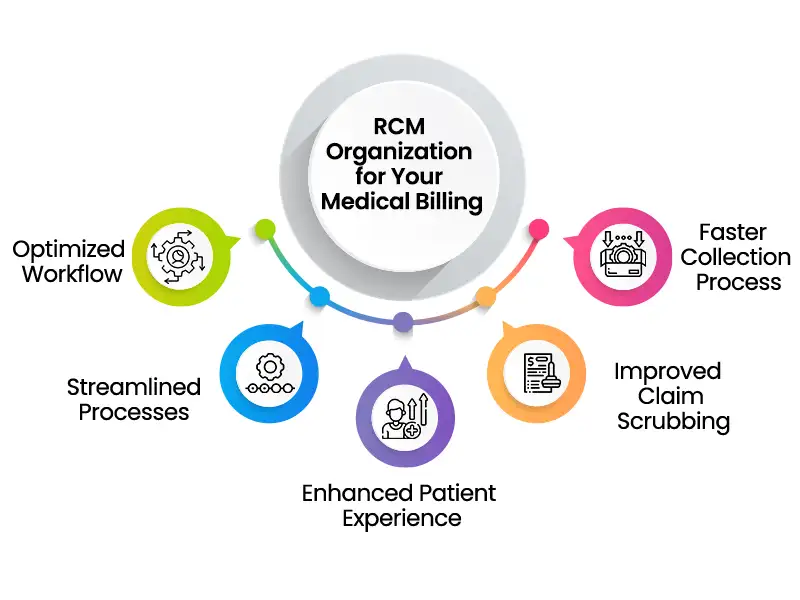
Revenue Cycle Management (RCM) is each step of the claim lifecycle. It works at the functional core of a medical care association as it covers the whole range of an office’s tasks, from front desk and scheduling, eligibility verification, care delivery, documentation, anesthesia medical billing and coding, and claim processing. The principal objective of RCM is to enhance the productivity of a medical care facility via automating manual process and diminishing the expenses of making collections.
The Advantages of Working With an Accomplished RCM Organization for Your Anesthesia Medical Billing Needs
The Most Common Challenges with Anesthesia Billing and Reimbursement and How an RCM Partner Can Help Overcome Them

Anesthesia Billing is more confounded than billing for most other medical fields. Between time units, modifiers, and other anesthesia codes in Medical Billing, it tends to be provoking for offices to comprehend how to deal with these intricacies nevertheless boost revenue. The following are the parts of the overall equation and interesting elements utilized for calculating anesthesia charges:
Base units – These mirror the intricacy of the surgery. Every strategy has a relating code with a base unit esteem. More troublesome systems that require a higher expertise level will have a higher base unit.
Time units – A period unit is typically 15 minutes long, however the valuation can change by contract. Time builds while the physician expects patient consideration, and stays in participation really focusing on the patient until the patient is at this point not under their consideration, and the report has been finished.
Changing units – Emergencies and certain circumstances in a patient’s health are considered changing units. Modifiers are pointers that will assist with distinguishing important details on a claim. Precise utilization of modifiers will assist with guaranteeing legitimate claims payment. Modifiers likewise assist with keeping away from copy charging and unbundling.
Contracted rate – This rate alludes to the legally settled upon amount between the anesthesiologist and insurance provider.
To guarantee appropriate repayment for anesthesia services, billers should include:
- Number of minutes of anesthesia organization
- Method anesthesia codes (00100-01999)
- Modifiers (e.g., modifier codes for actual status)
- Appropriate distinguishing proof by including any performing provider(s) NPI on the claim form.
Finding a Reputable Revenue Cycle Management Company for Your Anesthesia Medical Billing Needs
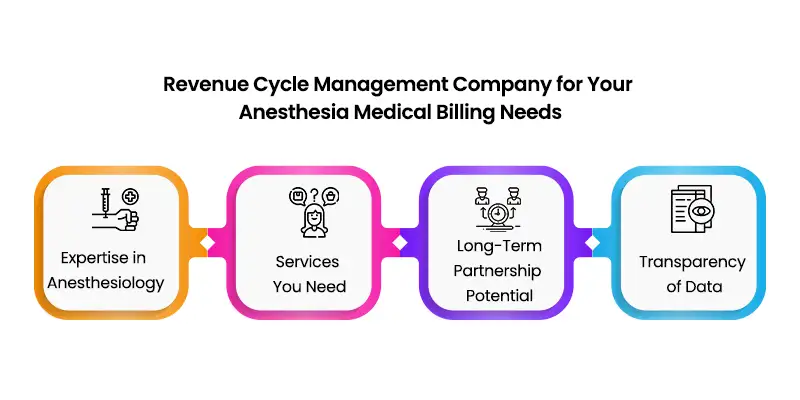
Expertise in Anesthesiology
Services You Need
Revenue cycle management ought to be taken care of by specialists who are know all about all parts of Anesthesia Medical Billing services. You should recognize your assumptions regarding which undertakings you need to regulate in your facility and which services you need the charging organization to give.
Long-Term Partnership Potential
Transparency of Data
How an Outsourced Billing Service Like MHRCM Health Can Streamline Your Anesthesia Billing and RCM

MHRCM will take a gander at each piece of your billing process as a chance to increase revenue by distinguishing and afterward rectifying the underlying driver of any issue. We comprehend how medical billing and collections are basic to the endurance and development of your facility, and patient assortments can turn into an overwhelming errand for your staff.
Let’s Work Together to Build the Best Revenue Cycle Management System
FAQ's
How Are Anesthesia Services Billed?
What Is The RCM in Medical Billing?
About the Author





