By Leo John
Do you want to enhance your Healthcare Revenue Cycle Management to the next level? Our unique approach with innovative strategies focuses on achieving financial stability and growth in the healthcare industry. If you’re a healthcare administrator or billing professional, we help you to analyze areas of improvement and execute effective RCM solutions. Our solutions facilitate simplifying your process, reducing errors and increasing revenue. In this blog, MHRCM discusses detailed descriptions and provides tips to optimize Revenue Cycle Management.
The Healthcare Revenue Cycle Optimization Checklist

Begin the Schedule in the Middle of the Day:
Technological Advancement in Healthcare Revenue Cycle Management
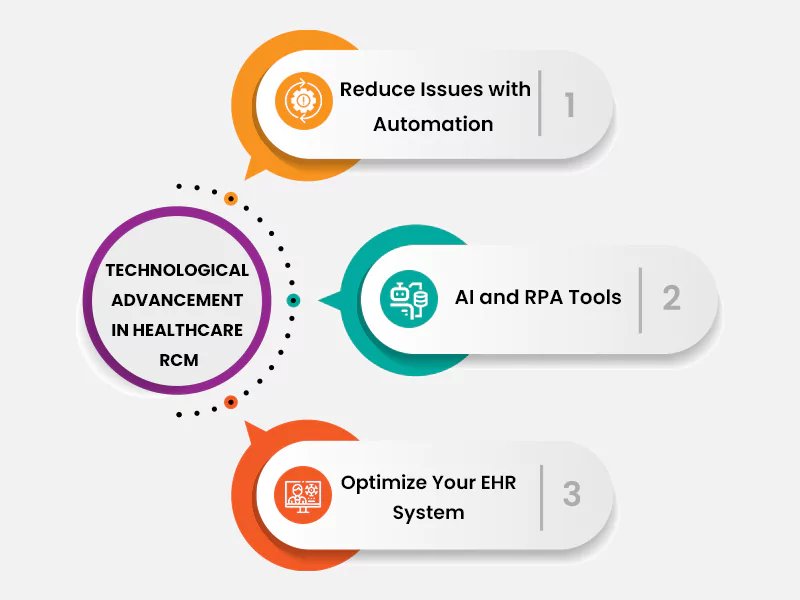
There are several components involved in the revenue process of Healthcare Service Provider. You need to identify which part of the Healthcare Revenue Cycle Management your administrative staff tend to prefer for payment. Look for ways to automate these areas of improvement and reduce issues. Consider specific areas like front-end access, Claims management, contract and cash application management. With the presence of an online client portal, Staff members are not be needed to handle scheduling and other conversations. Many facets of patient billing and refund claim processes can also be managed by automated systems.
With the goal of maximizing revenue, health care providers must assess their revenue management strategies and optimize their operations. Healthcare companies can build an effective team, manage receivables, streamline the claims process, be prepared for audits, and much more by implementing this article’s checklist to reality.
Develop Clinical Documentation Integrity (CDI) Team
Clinical Documentation Integrity is a significant factor of Healthcare Revenue Cycle Management. CDI includes capturing, documenting and reporting patient information. It focuses on ensuring clear documentation of patient medical records. CDI has many significant consequences for healthcare providers and is essential for Healthcare Revenue Cycle Management. The ultimate aim of the CDI team is to support other clinicians with the specified conditions for timely coding.
CDI experts play an important role in bridging the gap between healthcare providers, clinical staff and coding expertise. CDI expertise must have clinical, nursing, and medical coding backgrounds. The objective is to reflect the severity of illness, complexity of care and utilized resources. The following are benefits of CDI:
Denial Management Services Offered

medical billing involves our Denial Management Team with expertise. They analyze the reason behind denied claims and rectify issues. Resubmit the requests to the company and file appeals when necessary. Our team of experts understand that each case is unique. They focus on invalid medical codes and offers supporting documentation. Our team members validate all clinical information once again before re-submission.
Different factors within the Healthcare Revenue Cycle Management can lead to claim denials. Hence you need to analyze the trends in claim denials and develop a plan to reduce them based on the causes.
MHRCM has given detailed insights on the checklists for optimizing Healthcare Revenue Cycle. You can improve the financial performance of your business by providing transparent patient experiences. Our Revenue Cycle Management Services help to maximize revenue but deliver efficient results. For more information, visit the blog.
Frequently Asked Questions
About the Author





